Table of Contents
What is a Bunionette?
You may be more familiar with a bunion which involves the great toe drifting towards and sometimes overlapping with the little toes. There can also be a somewhat similar situation that can occur on the outside of the foot involving the fifth toe. This is called a bunionette. A bunionette is also known as a Tailor’s bunion. The term was coined centuries ago when tailors sat all day in a cross-legged position and their little toe was on the ground.
A bunionette is a deformity at the base of the fifth or little toe (see above diagram), which tends to occur gradually over time. Oftentimes, this does not cause any symptoms. There just might be a callous (thickened bump of skin) present. Some people with bunionette deformities experience localized pain on the outside aspect of the base of the fifth toe. This may be due to the altered walking mechanics associated with the poor toe alignment or due to that area rubbing against the shoe. There may also be a callous and pain on the other side of the toe where the fifth toe rubs on the fourth toe. With time, the bunionette may worsen; the fifth toe will tend to move inward towards the fourth toe and the attached long bone of the foot (the metatarsal) moves outward1. If you have ongoing pain or are at higher risk of infection due to broken skin (especially if you have diabetes), it is good to seek a formal diagnosis from a trusted podiatrist.2
A podiatrist’s physical examination will show a deformity of the fifth toe with a prominence on the outside at the base. The fifth toe itself usually has a normal range of motion up and down. The sensation and blood supply of the foot are typically normal1. There can be swelling in this area representing irritation of the bursa (a normally occurring fluid-filled sac). This swelling may change in size from day to day due to inflammation and is typically aggravated by tight shoes.
You probably won’t feel pain if you are barefoot or wearing sandals or flip-flops. Most bunionette deformities are caused by an inherited problem with the structure of the foot that is aggravated by poor choices of footwear3. Specifically, wearing footwear that constricts the forefoot such as high-heels or shoes with narrow, pointed toe boxes (front of the shoe encompassing the toes) are the biggest risk factor for developing a bunionette. Bunionettes are more common in women than in men, although cowboy boots can be blamed for the deformity in both men and women2.
Treatment Options
Most cases of bunionette deformity can be managed non-operatively. Non-operative treatment includes the following options:
Proper shoe wear:
Comfort pads

Toe Spacer

Behavioral Changes and/or Physical Therapy
If the deformity is severe enough, it may be necessary to limit the amount of time that the individual stands or walks1. This is, of course, a temporary situation to decrease the pain caused by the strain in this area. Physical therapy may be recommended and prescribed by the podiatrist; physical therapy can help to decrease inflammation with hands-on techniques as well as by balancing any other foot or lower extremity conditions that are contributing to the excessive stress at the bunionette site.
If the deformity is severe enough, it may be necessary to limit the amount of time that the individual stands or walks1. This is, of course, a temporary situation to decrease the pain caused by the strain in this area. Physical therapy may be recommended and prescribed by the podiatrist; physical therapy can help to decrease inflammation with hands-on techniques as well as by balancing any other foot or lower extremity conditions that are contributing to the excessive stress at the bunionette site.
Icing
Over-the-Counter Oral Medications
Surgery
In a small percentage of patients, operative treatment will be beneficial. Surgery will not be recommended if you have poor circulation, uncontrolled diabetes, if you are a chronic steroid user, or if you smoke cigarettes4. Surgery should only be considered after nonoperative management has failed (including but not limited to physical therapy, medications, change in shoe wear, pads and other inserts, rest, and weight-bearing limitations as needed). The type of operative treatment is dependent upon the actual deformity. Operative options for treating bunionette deformities include:
A. If you have a painful prominence without a bony growth, the typical surgery involves removing the painful soft tissue of the little toe3.
B. If you have an enlarged bump at the outer end of the fifth metatarsal head (where the toe meets the foot), then sometimes, a podiatrist may recommend the removal of the prominent bone on the outer aspect of the fifth metatarsal head. In some individuals with a bunionette deformity, the outside aspect of the fifth metatarsal head is prominent and simply removing this will help the symptoms.
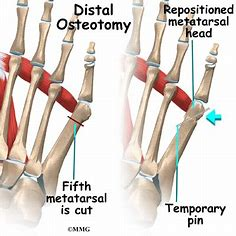
C. Cutting and repositioning the fifth metatarsal bone: In most patients with significant bunionette deformities, there is an increased angle between the fourth and fifth metatarsals (the long bones of the foot which connect to the toes) with the subsequently increased deformity at the fifth toe (metatarsophalangeal) joint. In these individuals, a formal cutting and repositioning of the bone (osteotomy) of the fifth metatarsal is necessary. This will allow the fifth metatarsal to straighten out. The bone may be held straight with a steel wire, screw, or plate and screws, depending upon the surgeon’s preference. Depending upon the exact nature of the deformity, the bone can be cut close to the bunionette or further up the foot to reposition the entire bone. These procedures are combined with a soft tissue tightening of the outer (lateral) joint capsule of the fifth metatarsophalangeal joint, further correcting the deformity1.
Surgery is performed to realign the bone so that it does not point outward. This is usually performed as an outpatient procedure, which means you can go home the same day as the surgery, but it can have a long recovery period3. Your surgeon will explain which surgery type and why is needed, usually coordinating with the relative “size” of the bunionette3.
After the surgery, you will likely be placed in a surgical shoe or possibly a walking boot until the surgeon clears you to begin walking in a gym shoe. Elevation above the heart is usually indicated for the first few days to assist with decreasing swelling. Your stitches are usually taken out or dissolve 2-3 weeks after surgery. You will be asked not to soak your foot or get your surgical area wet until the surgical wound is healed and closed. Your doctor will likely prescribe physical therapy to restore your range of motion, strength, and to facilitate a full return to your desired activities. Most bunionettes do not come back after being treated with the right type of surgery. The surgery should correct the underlying cause of the problem. However, wearing shoes that are too narrow, such as those with a pointed toe box can still cause irritation and inflammation at the operated little toe3.
If you are concerned about your bunionette, feel free to make an appointment with one of our knowledgeable podiatric surgeons to find out about what type of treatment may be right for you.
- Stavrou, Peter, MD. Bunionette. Foot Education, November 24, 2018.
- Cluett, Jonathon, MD. What is a bunionette? Verywell Health, 05/24/2022.
- Haddad, SL. Bunions. American Academy of Orthopedic Surgeons. Updated 2/2016.
- Aydogan, Umur. Bunionette Deformity Correction. American Orthopaedic Foot & ankle Society.

Meet Weil Foot & Ankle Institute
By: Weil Foot & Ankle Institute, Published: May 5, 2023
Review By: Bilal Siddiqui DPM – Jun 12th, 2023


