Table of Contents
Bunions (medical term hallux valgus) are the most common surgical procedure performed by foot surgeons. It is estimated there are 330,000 bunion procedures performed annually in the United States. There are hundreds of procedures which have been developed and modified over the years to correct bunion deformities.
How Are Bunions Corrected?
One of the most utilized bunion correction procedures in 2022 is the Lapiplasty procedure. While the Lapiplasty procedure is an innovative new procedure involving specific instrumentation, it is based on the Lapidus bunion procedure first utilized in the 1930s. Essentially the Lapidus procedure is a bunion correction incorporating an arthrodesis or fusion [making 2 bones into one bone] of a joint [the first tarsometatarsal joint] on the inside of the foot. Dr. Lapidus performed the first truly original Lapidus operation on April 8, 1931. As he was the one to popularize the procedure, it bears his name without he himself claiming originality as the procedure was initially advocated twenty years earlier in 1911 by Dr. Albrecht.
Do I Need Surgery For My Bunions?
Before we talk about the specifics of the Lapiplasty procedure itself, we need to talk about bunions in general. Bunions are extremely common. Research indicates that 23% of people aged 18 to 65, and 36% of those older than 65 have bunions.
However, do all bunions need surgery? The answer is not all bunions. Only painful bunions which do not respond to an initial conservative care protocol require surgical correction. Conservative care for bunions includes change of shoe gear to wide or open toe shoes, use of toe spacers or bunion splints, and use of functional inserts or custom orthotics. Once conservative care options are exhausted and the bunion continues to cause pain, patients should then consider electing to have bunion correction surgery performed.
Patients always ask “Doc, do I need bunion surgery?”. My answer is always “You tell me, I don’t tell you!” In my opinion patients should elect for bunion surgery when they can’t wear the shoes they need to wear or want to wear, or can’t do the activities they need to do or want to do.
Once the decision for surgery is made, your surgeon will recommend a surgical option or options to correct your bunion. This recommendation will depend on several factors:
- how large the bunion is on weight bearing (standing) x-rays
- how severe the bunion misalignment is
- whether the bunion is related to osteoarthritis
- how loose the bunion and/or foot is
How Does the Lapiplasty Procedure Work?
This gets us back to the Lapiplasty procedure. We now know what a Lapidus procedure is, but what about the ‘plasty’ part? Plasty means to mold, graft or form a body part. Therefore the designers of the Lapiplasty procedure chose the name based on the procedure using the Lapidus concept and molding [correcting] the bunion of the foot.
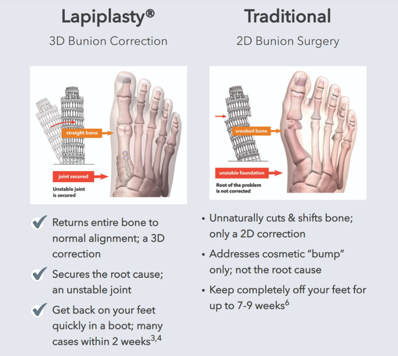
In 2014, a group of five physicians specializing in foot surgery met in Memphis, TN and unanimously identified bunion correction as an unpredictable and frustrating surgical procedure. They concurred that bunion surgery was unreliable, unpredictable, and had a high recurrence rate. In addition, recent research they were aware of indicating a previously underreported presence of excessive bone rotation [pronation] occurring with bunions was not being addressed with traditional bunion surgery. This led to the idea of correcting bunion deformities in three planes, or a three-dimensional 3D bunion correction. With this, the Lapiplasty procedure was developed. The procedure utilizes specific instrumentation and fixation to provide a reproducible bunion procedure with complete correction of the deformity in all three planes with low risk of bunion recurrence.
Every physician who performs the Lapiplasty procedure goes through a specialized training program in order to perform the procedure. This provides standardization for the procedure to provide consistent reproducible results, no matter the surgeon performing the procedure. The procedure is performed through a stepwise approach which allows for efficient reliable complete correction of the bunion.
So how does the Lapiplasty procedure provide this reliable reproducible consistent 3D bunion correction? For the answer to this question, the following information was obtained directly from the lapiplasty.com website:
First, Lapiplasty™ has a novel “positioning” instrument that allows the surgeon to quickly and reliably reposition and hold the metatarsal in 3-planes before making any bone cuts. Next, the surgeon uses a guide to make precise and accurate cuts to the joint surfaces. Freehand variability is simply out of the equation.
- Independent Survey, June 2020
- AOFAS Member Survey Aug 2021
- Ray J, et al. Foot Ankle Int. 2019 Aug;40(8):955-960
- Dayton P, et al. J Foot Ankle Surg. 2019. 58:427-433
- Dayton P, et al. J Foot Ankle Surg. 2020, 59(2): 291-297
- Park CH, Ahn JY, Kim YM, Lee WC. Int Orthop. 2013 Jun;37(6):1085-92
Once a patient decides they would like to elect for surgical correction of their painful bunion deformity, the recommendation to perform a Lapiplasty procedure is based on several factors obtained through a visit with your surgeon where weightbearing x-rays are obtained.
The Lapipasty procedure is indicated for bunions with one or all of the following characteristics:
- moderate to severe size bunion on weight bearing (standing) x-rays
- misaligned rotation of the first metatarsal
- a “loose” foot or bunion, medically referred to as “hypermobility”
The Lapiplasty procedure is performed as an outpatient procedure in a hospital or surgery center. A combination of monitored anesthesia care (twilight sleep) and local anesthetic injected into the foot is used for the procedure. Once the procedure is completed, a bandage is applied to the foot which is not removed until an initial post-operative visit one to two weeks after the procedure.
What Is Post-Procedure Care Like For A Lapiplasty?
Initially there is a period of non-weightbearing where no weight is allowed on the foot. This occurs from after surgery until x-rays are obtained at the initial post-operative visit. Crutches or a knee scooter is used to keep weight off the foot during this important time of post-surgical healing of your incision and the bone. If these initial x-rays reveal appropriate signs of bone healing, progression to the use of a below the knee walking boot is allowed. At four weeks after surgery, physical therapy is initiated. Progression out of the below the knee walking boot and into an athletic shoe occurs at four to six weeks after surgery. Non-impact type athletic activity such as swimming, biking, walking, or use of the elliptical machine for exercise begins six to eight weeks after surgery. Running is allowed three to four months post-surgery. It takes approximately four to six months until there is full recovery from surgery. This is accomplished when the pre-surgical pain has resolved, post-surgical foot swelling has resolved, and the strength and range of motion to the foot and ankle have returned to normal.
Physical therapy is an important part of the post-surgical protocol after the Lapiplasty procedure to regain strength and range of motion of the foot and ankle after the Lapiplasty procdure. Physical Therapy Begins at week four and encompasses two phases.
Phase I:
- First visit consists of an evaluation, treatment with gentle first metatarsophalangeal joint mobilization/range of motion, gait training, modalities as needed, and a home exercise program. The home exercise program includes first metatarsophalangeal joint plantar flexion mobilization/strengthening.
- Treatment during this time includes first metatarsophalangeal joint plantar flexion strengthening with a hallux control strap or light resistance theraband and range of motion/self-mobilization of the first metatarsophalangeal joint.
- Goal: maximize first metatarsophalangeal joint strength and range of motion, especially into flexion.
- Treatment will remain non-weightbearing on the treatment table and sitting for the first four weeks of physical therapy with a focus on great toe metatarsophalangeal joint range of motion and strengthening.
- Range of motion and strength are included with other joints as needed except that cuneiform/metatarsal joint mobilization is not allowed due to the surgical fusion to this joint performed with the Lapiplasty procedure.
Phase II:
- Progress to full weightbearing in gym shoe by week six
- Full weightbearing/gait training: focusing on full first ray contact during appropriate phases of gait with shoes. Begin to roll through the first ray, with emphasis on proper great toe extension and pronation.
- May begin standing heel raises at week eight when ready to do so.
- Begin closed kinetic chain strengthening and balance activities.
- Progress as able – return to all functional activities and start preparing for return to sport/running.
To finalize, here is an example of a patient with a painful bunion who had surgical correction via Lapiplasty procedure:
Info: Thirty-six-year-old female. Chronic bunion pain caused by a hallux valgus deformity. Pain over the last year, where conservative care including wide shoe gear, inserts, bunion splints, and toe spacers was not effective. Before and after weightbearing [standing] x-rays reveal correction of the bunion deformity with a decrease in the width of the foot after Lapiplasty surgical correction. As seen in the radiographs, the Lapiplasty procedure utilizes two low profile plates and up to eight to nine screws to maintain the correction.



Meet Weil Foot & Ankle Institute
By: Weil Foot & Ankle Institute, Published: Dec 13th, 2022
Review By: Jeffrey Baker DPM – Feb 14th, 2023


